
Sweat, Sunscreen, and Acne: How to Stay Clear Through Spring Activities
Think skin exams are only for those with visible concerns? Annual skin checks can detect early signs of cancer.
As winter wraps its chilly fingers around us, many experience the familiar discomfort of cold hands and feet. However, for some, this discomfort goes beyond the usual winter woes and signals a condition known as Raynaud’s syndrome. As many as five percent of the United States population suffers from Raynaud’s, with 80 percent of those affected being women.
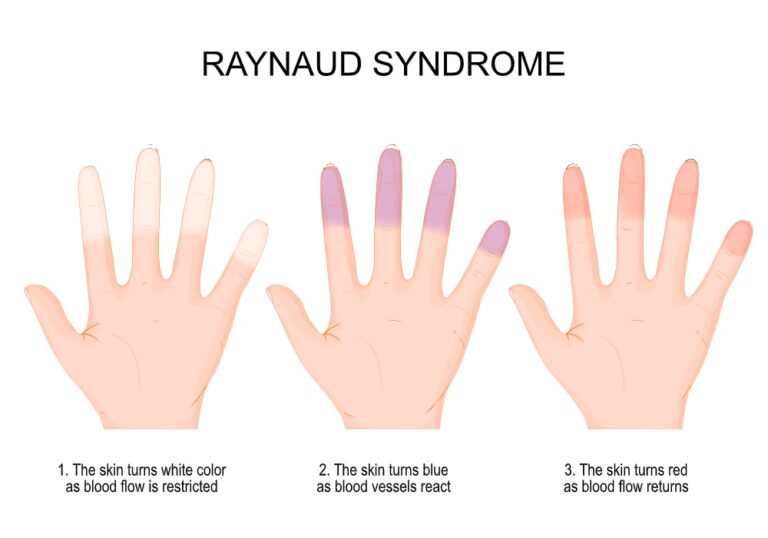
Raynaud’s syndrome can cause fingers and toes to turn white, blue, and red, accompanied by numbness and tingling. Understanding and managing this condition can significantly improve your quality of life. This article will guide you through everything you need to know about Raynaud’s, including its causes, symptoms, and effective treatments. Whether you’re seeking to understand your symptoms better or looking for advanced care options, we’ve got you covered.
While this article spells out some important information about Raynaud’s syndrome, we highly recommend you read the full article, here are the key points we will focus on:

Raynaud’s is more than just a reaction to cold temperatures; it’s a condition that can significantly affect your daily life. Let’s delve into what Raynaud’s entails and why it’s crucial to distinguish between its different forms.
A healthy circulatory system ensures blood flows freely to all body parts, supplying vital oxygen and nutrients. However, for individuals with Raynaud’s, this process is disrupted. The condition causes an exaggerated response to cold or stress, narrowing small blood vessels in the extremities. This results in a temporary reduction of blood flow, primarily affecting fingers and toes. The physical signs may include the affected areas turning white as blood flow is restricted, followed by the skin turning a bluish color as the blood vessels react, and finally the affected areas may turn red as the blood flow returns.
During the colder months, reports of numbness, tingling, and cold extremities increase, but not all these symptoms necessarily indicate the same type of Raynaud’s. It’s essential to understand the difference between Raynaud’s disease and Raynaud’s phenomenon for proper management and treatment.
Raynaud’s Disease vs Phenomenon
This form occurs independently of other diseases. It’s the more common and less medically severe version. The cause is largely unknown, but is thought to be related to how the nervous system controls blood vessel dilation and constriction. Symptoms can often be managed with lifestyle changes and self-care measures.
This form is less common but more severe and is associated with other medical conditions, such as autoimmune or vascular diseases. Secondary Raynaud requires addressing the underlying conditions to effectively manage symptoms and prevent complications.
Understanding which type of Raynaud’s you have is crucial for effective treatment. While primary Raynaud’s can often be managed with simple lifestyle adjustments, secondary Raynaud’s may require more comprehensive and advanced medical intervention.
While the exact trigger for Raynaud’s can vary, distinguishing between primary and secondary Raynaud’s helps identify the potential causes.
Studies show that Raynaud’s symptoms, particularly in its secondary form (phenomenon), are often a manifestation of underlying health issues, many involving the immune or circulatory systems. Recognizing these causes is crucial for patients and healthcare providers to manage the condition effectively.
Primary Raynaud’s Disease’s specific causes may be unclear, but certain factors are well-recognized as its triggers, such as:
Raynaud’s Phenomenon or Secondary Raynaud’s is linked to various medical conditions, primarily affecting connective tissue or the autoimmune system. These include:
For individuals experiencing symptoms of Raynaud’s, it is essential to get checked out by a dermatologist. Specialists at Bryn Mawr Dermatology are equipped to determine whether you have primary or secondary Raynaud’s and can provide personalized management plans to help control symptoms and improve overall health.
Diagnosing Raynaud involves a combination of clinical evaluation and diagnostic tests to distinguish between primary and secondary forms of the condition. Physicians aim to understand the full scope of symptoms and any potential underlying causes.
Key Factors in Diagnosing Raynaud’s:
Identifying the right time to seek medical advice for Raynaud’s is critical for effective management. Here are clear indicators for when a dermatologist’s expertise is needed:
A timely visit to a dermatologist, such as the team at Bryn Mawr Dermatology, is essential for accurate diagnosis and personalized treatment planning.
Bryn Mawr Dermatology stands at the forefront of treating Raynaud’s, offering personalized care and advanced treatment options. Our team is dedicated to providing a comprehensive approach to managing your symptoms effectively. Unlike other practices, we prioritize understanding your unique condition and crafting a tailored treatment plan.
If you’re navigating the challenges of Raynaud’s, let Bryn Mawr Dermatology guide you towards a comfortable, symptom-free life. Schedule an evaluation today to explore your treatment options. Our state-of-the-art facilities and compassionate team ensure a welcoming environment from the moment you enter. Begin your journey to improve your health by calling (610) 525-7800. We’re here to provide the care you deserve. By choosing Bryn Mawr Dermatology, you’re not just getting treatment; you’re gaining a partner in your healthcare journey, dedicated to improving your quality of life.

Think skin exams are only for those with visible concerns? Annual skin checks can detect early signs of cancer.

Think skin exams are only for those with visible concerns? Annual skin checks can detect early signs of cancer.

Think skin exams are only for those with visible concerns? Annual skin checks can detect early signs of cancer.

Think skin exams are only for those with visible concerns? Annual skin checks can detect early signs of cancer.

Discover a youthful lift without surgery. Learn how our thread lift at Bryn Mawr Dermatology can rejuvenate your appearance.

Discover a youthful lift without surgery. Learn how our thread lift at Bryn Mawr Dermatology can rejuvenate your appearance.

By: Bryn Mawr Dermatology, Published: Feb 12, 2024
Medically Reviewed By: Christine Stanko, MD, FAAD – Feb 12, 2024
For COSMETIC APPOINTMENTS:
For MEDICAL APPOINTMENTS: